Nursing Home Safety During COVID: PPE Shortages
Seven months into pandemic, 20 percent of facilities lacked enough supplies
Downloads
PennPIRG Education Fund
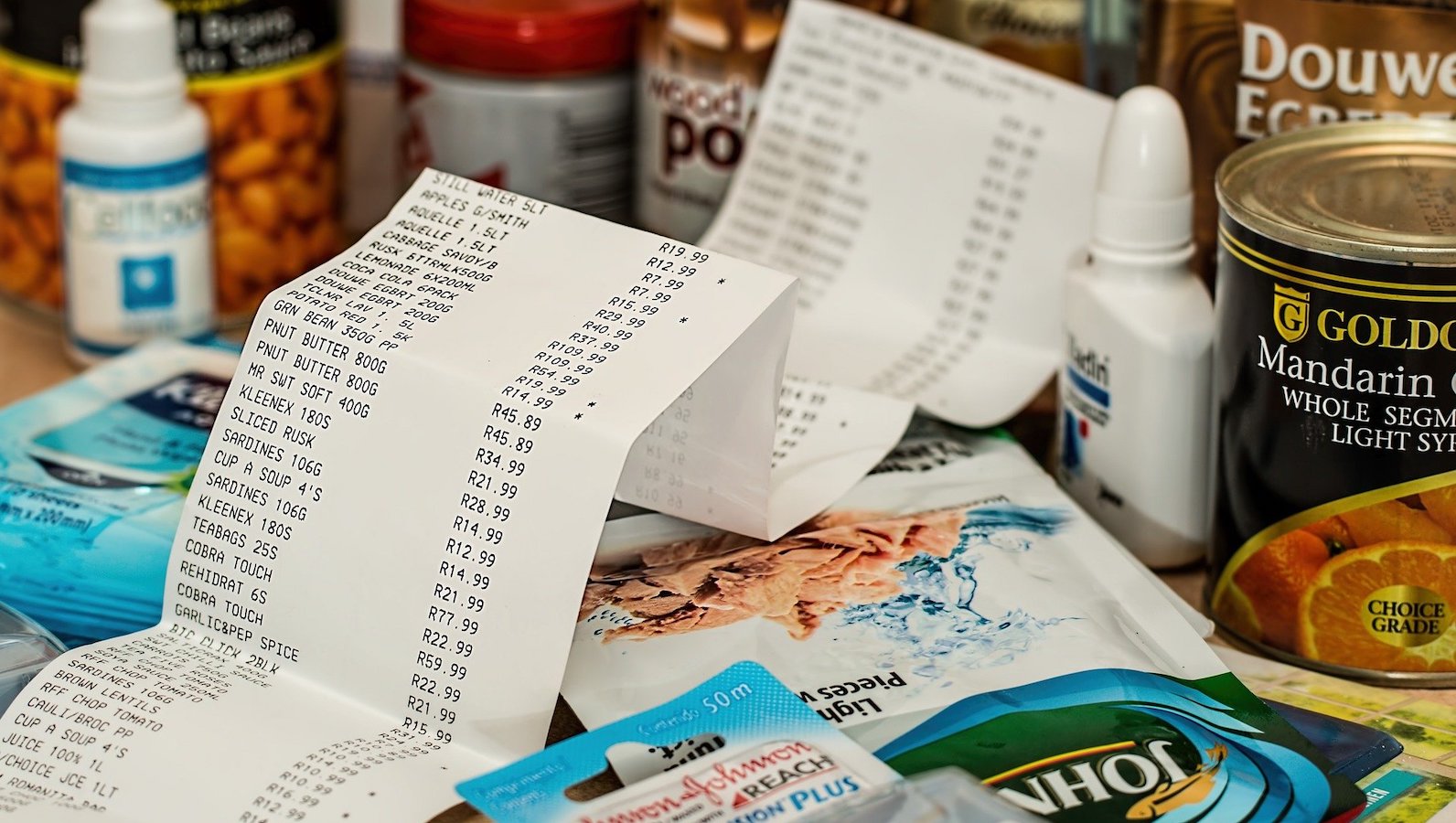
Thousands of nursing homes nationwide are dealing with horrific short- ages of masks, gowns and other items they need to protect residents, workers and the broader community from COVID-19. And seven months into this pandemic, the short- ages have actually become much worse.
At any given time, about 1.3 million people1 with long-term medical issues or short-term rehabilitation needs are residing in the na- tion’s 15,000 nursing homes.2 And too many of them are at risk, according to an analysis of government data by the U.S. PIRG Edu- cation Fund and Frontier Group.
As of late August, 226,495 residents in 2,981 nursing homes3 nationwide were at risk because the homes had dangerously low supplies of one or more types of personal protective equipment (PPE) such as N95 masks or gowns, according to data submit- ted to the federal government. That means that 20 percent4 of nursing homes in late August had a less-than-one-week supply of one or more types of PPE, which represents a critical shortage by industry standards.
Of those, 96,132 residents in 1,244 nursing homes5 nationwide were at severe risk because the homes were completely out of one or more types of critical personal pro- tective equipment (PPE) such as N95 masks or gowns. Our analysis looked at data submitted to the Centers for Medicare & Medicaid Services (CMS)6 from May 2020 (when the submissions started) through August 2020.
The shortages actually became more grave as the summer went on, with three times7 as many nursing homes reporting they were completely out of masks, gowns and eye protection in late August, compared with mid-July.
The problem of PPE shortages spanned the entire three-month period we analyzed. Amazingly, 20 percent8 of nursing homes reported they were completely out of one or more types of PPE at some point from late May through late August. In addition, 46 percent9 of all nursing homes nationwide reported they didn’t have a one-week sup- ply of at least one type of PPE at some point from May through August. A one-week sup- ply is considered the minimum acceptable.
“In the midst of an outbreak, it would be very easy to burn through that remaining supply in less than a week,” said Brian McGarry, Ph.D., assistant professor of geri- atrics/aging and public health sciences at the University of Rochester Medical Cen- ter.10 In addition, a home may have no idea when its next shipment of PPE may arrive. Homes with less than one week’s supply may start rationing, forcing workers to re- use PPE or go without, McGarry said.
One of the many questions this analysis raises: How did the PPE situation not improve and actually get worse throughout this year, as the seriousness of the pandemic became obvious?
In January, the U.S. government declared a public health emergency11 in response to the global threat from the coronavirus. The virus was known to be highly contagious and be transmitted through the air. There was wide- spread fear a pandemic would sweep through
the United States, causing people of all ages to become potentially extremely ill. Sick people often need medical care. Health care work- ers protect themselves from transmittable diseases, especially severely contagious ones, with masks, gloves and other PPE.
Yet seven months after the public health emergency declaration, this nation was still experiencing dangerous shortages of PPE.
Topics
Find Out More


Another winter during COVID-19: How to stay safe and sound

Nursing home safety during COVID: Cases and Vaccines